Abstract
Introduction: Myeloid-derived suppressive cells (MDSC) are an heterogeneous group of immature myeloid cells with strong immunosuppressive activities which made them of particular interest in the context of allogeneic stem cell transplant (Allo-SCT). In mice models, MDSC modulate the function of alloreactive T cells and prevent graft versus host disease (GVHD) without impairing graft versus leukemia (GVL) effect. Data are limited in humans, but higher proportions of MDSC in the graft seem to protect against both acute and chronic GVHD. However, the influence of circulating MDSC is not fully explored especially regarding their impact on post-transplant GVL effect and survivals. Here we focused on the role of peripheral levels of monocytic-MDSC (mMDSC) in a cohort of adults with acute (both myeloid or lymphoid) leukemia (AML or ALL) having received Allo-SCT.
Methods: This prospective monocentric study aimed at documenting the impact of the percentage of mMDSC before and after allo-SCT in terms of incidence of acute and chronic GVHD, overall (OS) and leukemia-free (LFS) survivals, (grade 3/4 acute or extensive chronic) GVHD-free relapse-free survival (GRFS), relapse and non-relapse mortality (NRM) in a cohort of ALL or AML patients (pts). Inclusion was performed after informed consent at diagnosis as part of a more global study (Abstract ASH 2021 # 3465), pts who were ultimately transplanted being included in this sub-group analysis. mMDSC were defined by the minimal CD14+/CD11b+/CD33+/HLA-DR-/low immunophenotypic pattern, at variance from granulocytic MDSC that lack CD14 and express bright CD15. Cells were assessed in a lysis-no-wash flow cytometry technique using peripheral blood collected on EDTA before conditioning then at day+60 post-transplant. Data acquisition was performed on a Navios® flow cytometer (Beckman Coulter, Miami, FL). mMDSC were expressed as a percentage (%) of total nucleated cells defined as CD45+. The study was registered at the French Commission Nationale de l'Informatique et des Libertés as CNIL 2016-038 and approved by the Ethic Review Board of Nantes University Hospital.
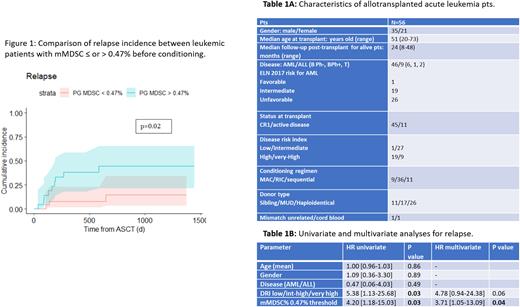
Results: Among 73 AML and 14 ALL pts included at diagnosis, 47 and 9, respectively, were ultimately allografted between February 2018 and October 2021. Pts characteristics are provided in Table 1A. The median follow-up for alive pts from Day 0 was 24 months (range: 8-48). Considering the whole cohort, 2-year OS, LFS and GRFS were 61.9+6%, 55.9+7% and 32.4+6%, respectively, while 2-year NRM and Relapse incidence were 11+4% and 29.6+6%.
In pre-graft, 46 pts were evaluated at a median of 20 days from Day 0 (range: 6-83). The median % of mMDSC was 0.45% (range: 0-11.85) with no differences between AML and ALL (p=0.32). The best cut-off assessed by ROC analyses was 0.47%. According to this value, the incidence of cytologic relapse at 2 years was significantly higher in pts with >0.47% of mMDSC (14.5+8% vs 44.4+11%, p=0.02, Figure 1) while no impact on survivals, NRM or GVHD was observed. Of note, the incidence of relapse was similar between AML and ALL (29% vs 37.5%, p=0.95). In multivariate analysis (Table 1B), higher pre-graft mMDSC % remained associated with higher risk of relapse (HR: 3.71; 95%CI: 1.05-13.09, p=0.04).
At day+60, 42 pts were evaluated. The mMDSC median level was 0.52% (range: 0-5.03) with no differences between AML and ALL (p=0.32). No best cut-off was determined. Survivals were similar between pts with ≤ or >0.52% of mMDSC at this time. It was also the case for incidences of relapse, NRM and chronic GVHD. However, the incidence of severe acute GVHD (grade 3/4) was significantly and paradoxically higher in the group of pts with >0.52% mMDSC (33% vs 5%, p=0.04) suggesting a possible amplification of immunosuppressive mMDSC as a reaction to GVHD since the median time of GVHD grade 2-4 occurrence was 30 days (range: 20-123) post-transplant.
Of note, the kinetics (increases or decreases of mMDSC %) between pre-graft and D60 had no influence on outcomes.
Conclusion: This prospective study demonstrates a negative impact of higher proportions of mMDSC before allotransplant in leukemic pts. This higher proportion is predicting relapse, suggesting a protective role and tolerance of tumoral cells by mMDSC themselves. This paves the way to therapeutic intervention to decrease the incidence of relapse in such pts.
Disclosures
Chevallier:Pfizer: Research Funding; Jazz Pharmaceuticals: Honoraria; Incyte: Research Funding; Takeda: Honoraria; Abbvie: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal